Abstract
Background: Symptomatic pseudarthrosis is one long-term complication in patients treated with anterior discectomy and fusion (ACDF). When revising a pseudarthrosis, a surgeon must decide to intervene posteriorly and/or anteriorly. Open posterior cervical fusion (PCF) is attractive for high rates of arthrodesis, however this technique introduces risks of added complications resulting from extensive soft tissue dissection. The purpose of this study was to assess long-term outcomes in patients undergoing tissue-sparing PCF with facet instrumentation to treat a single-level pseudarthrosis.
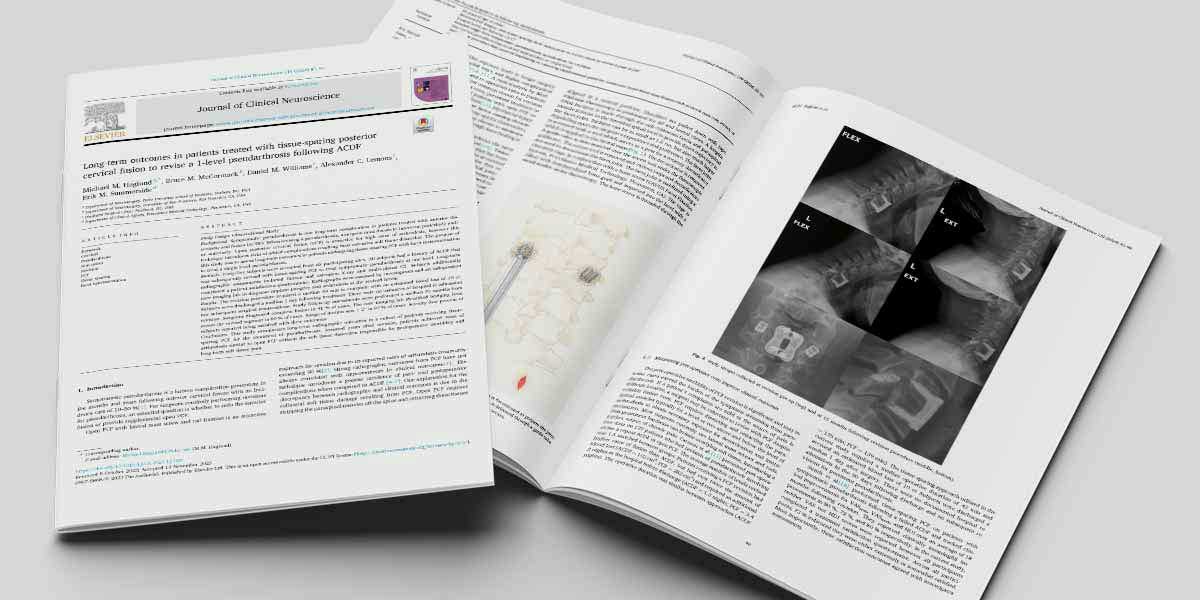
Methods: Forty-five subjects were recruited from six participating sites. All subjects had a history of ACDF that was subsequently revised with tissue-sparing PCF to treat symptomatic pseudarthrosis at one level. Long-term radiographic assessments included flexion and extension X-ray and multi-planar CT. Subjects additionally completed a patient satisfaction questionnaire. Radiographs were assessed by investigators and an independent core imaging lab to diagnose implant integrity and arthrodesis at the revised levels.
Results: The revision procedure required a median 49 min to complete with an estimated blood loss of 10 cc. Subjects were discharged a median 1 day following treatment. There were no instances of hospital re-admission nor subsequent surgical interventions. Study follow-up assessments were performed a median 39 months from revision. Surgeons diagnosed complete fusion in 91 % of cases. The core imaging lab identified bridging bone across the revised segment in 80 % of cases. Range of motion was < 2° in 93 % of cases. Seventy-four percent of subjects reported being satisfied with their outcomes. Conclusions This study summarizes long-term radiographic outcomes in a cohort of patients receiving tissue-sparing PCF for the treatment of pseudarthrosis. Assessed years after revision, patients achieved rates of arthrodesis similar to open PCF without the soft tissue dissection responsible for perioperative morbidity and long-term soft tissue pain.
Study Design: Observational Study
Author keywords: Cervical, Pseudarthrosis, Non-union, Revision, PCF, Tissue sparing, Facet instrumentation